- Home
- About us
- News
- Club 30
- About us
- News
- IX Naukowy Dzień Doktoranta
- Serdecznie dziękujemy za wsparcie
- KLUB 30 – warsztaty z (auto)prezentacji w dziedzinie medycyny
- KLUB 30 – warsztaty z przygotowania publikacji naukowych z zakresu medycyny (Proper Medical Writing)
- Wsparcie dla Agatki
- Akromegalia – optymalizacja leczenia
- Wsparcie leczenia córeczki naszej koleżanki.
- Warsztaty z wykorzystania AI w pracy naukowo-klinicznej endokrynologa oraz kompleksowego podejścia do leczenia choroby otyłościowej.
- Authorities
- Regulations
- Contact
- Archives
- Application form
- Science and education
- Membership fee
- Contact
 Polish Society of
Polish Society of
Endocrinology
Pasireotide treatment in giant prolactinoma resistant to dopamine agonists
24.03.2025
Maria Komisarz-Calik, Grzegorz Zieliński, Karol Ciszek, Anna Bogusławska, Alicja Hubalewska-Dydejczyk, Aleksandra Gilis-Januszewska
Giant prolactinomas (GP), defined as tumours > 40 mm, are a scarce subtype of lactotroph plurihormonal pituitary neuroendocrine tumours (PitNET) (accounting for 2–3%), occurring predominantly in young men. Treatment of GP is often challenging and requires a multimodal approach. Resistance to dopamine agonists (DA) is defined as a lack of normalisation of prolactin serum levels or lack of at least 30% reduction in maximum diameter of the tumour treated with standard dopamine agonist doses (7.5–10 mg/day of bromocriptine or 2.0 mg/week of cabergoline) for at least 6 months.
We present a case of a 17-year-old male with a DA-resistant GP treated with a second generation of somatostatin analogue-pasireotide LAR. In August 2022, the patient was admitted to the Endocrinology Department. He had been receiving cabergoline since 2020 and underwent 2 neurosurgical procedures in Ukraine (July 2020 and January 2021) due to severe headaches and vision disturbances. On admission, he complained of diplopia, temporal visual field deficits, persistent headaches (4/10 on the numerical rating scale [NRS]), presented with obesity, and symptoms of hypogonadism. Significantly elevated prolactin concentration [43.211 μlU/mL, reference range (RR): 86–324 μlU/mL], with decreased testosterone, low follicle-stimulating hormone (FSH), and luteinising hormone (LH) accompanied by thyroid-stimulating hormone (TSH) and free thyroxine (fT4) indicative of central hypothyroidism were detected. Magnetic resonance imaging (MRI) from July 2022 revealed a residual pituitary tumour (38 × 34 × 33 mm) infiltrating the right cavernous sinus and right optic nerve (Fig. 1AB). No heart valves abnormalities were found on echocardiography. The dose of cabergoline was increased to 3.5 mg/week. Levothyroxine (50 mcg/day) and testosterone injection (1×/2 weeks) were commenced. Due to high prolactin values (51,247 μlU/mL), cabergoline was uptritated to 4.5 mg/week. In May 2023, through the dopamine agonist resistance, a therapy with pasireotide LAR was implemented at the dose of 20 mg/month (increased to 40 mg/month after 6 months). After pasireotide commencement, the tumour dimensions stabilised (Fig. 1CD), and signs of tumour cystic degeneration occurred (Fig. 1EF). The patient reported remarkable headache alleviation (0/10 on the NRS scale), the appearance of facial hair, and body weight reduction. The ophthalmologic examination showed an improvement in the visual field. The prolactin level decreased to 35,000 μlU/mL (32% of the baseline concentration from September 2022).
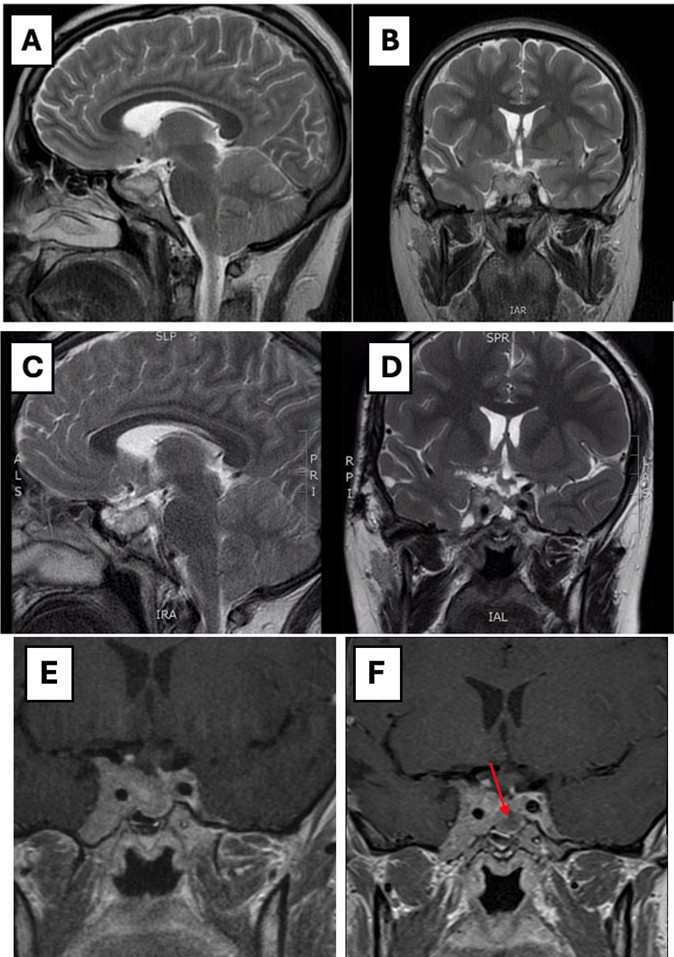
Figure 1A, B. Sagittal T2 (A) and coronal T2 (B) magnetic resonance imaging (MRI) (July 2022) showing pituitary tumour (38 × 34 × 33 mm) infiltrating the right cavernous sinus and right optic nerve; C, D. Sagittal T2 (C) and coronal T2 (D) MRI (July 2023) showing stable dimensions of the tumour after pasireotide implementation; E, F. Coronal T1 MRI (July 2022) and coronal T1 MRI (July 2024) comparing the part of the tumour without (E) and with (F) a cystic degeneration of the tumour (arrow)
Most GPs are benign; however, due to tumour dimensions, they might show aggressive behaviour, infiltrating the optic chiasm, sphenoid sinuses, or cavernous sinuses. GPs usually respond well to DA therapy; cabergoline is the most effective DA. Surgical treatment is indicated in pituitary apoplexy, cerebrospinal fluid leakage, and tumour growth despite optimal treatment. GPs are more often nonresectable and prone to postoperative recurrence; therefore, the surgeries are associated with significant mortality. Moreover, extracellular extension and cavernous sinus invasion (evaluated by Knosp classification) are associated with lower remission rates. The prognostic factor associated with early remission after transsphenoidal surgery was lower prolactin concentration on the first postoperative day. The current consensus is that temozolomide is usually recommended as a treatment option for aggressive prolactinoma with persistent growth. However, there is increasing evidence that pasireotide can be successfully introduced due to its potential antitumor and analgesic effect. This case emphasises that GPs require an individualised therapeutic approach. Pharmacological therapy with pasireotide in DA-resistant GPs should be regarded as the first-line treatment. Alleviation of headaches, decreased prolactin, tumour stabilisation, and cystic degeneration are considered satisfactory outcomes. Further studies should be conducted to evaluate the effectiveness of pasireotide in GPs.